The foot soldiers in India’s battle to improve public health
By Sameer Yasir
BAGDOLI — A health worker was making her daily rounds in a village in the northern Indian state of Rajasthan when the husband of a woman with shooting labour pains ran up to her.
For months, the health worker, Bhanwar Bai Jadoun, had been advising the woman to give birth at a hospital. But the woman’s mother-in-law insisted on delivering the baby at home with the help of a local midwife.
Now complications had set in. Jadoun suggested rushing the woman to a hospital 10 miles from the village, Bagdoli; she would notify the doctors there. An auto rickshaw was arranged. Mother and baby were saved.
“When people see me every day, they know they can trust me,” Jadoun said. “They consider me as their guide for a healthy life.”
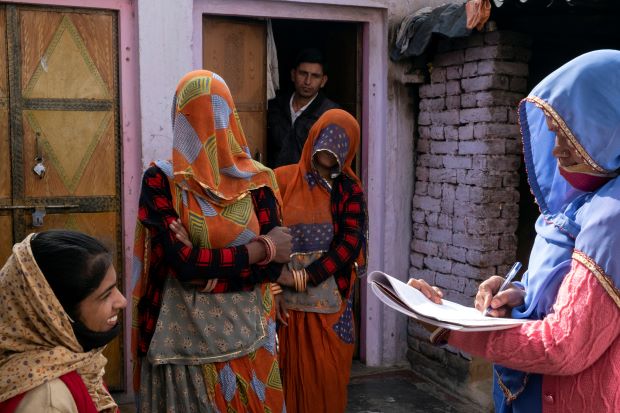
Over the past two decades, a government program has provided basic health care at the doorsteps of homes across India’s vast territory. Essential to the project is an army of more than one million female health workers, who trek through rugged terrain and dense jungles to treat some of India’s most vulnerable women and children, for little pay and sometimes at the expense of their own lives.
These women are neither doctors nor nurses, but they are given training to bridge the health care gap in places, both rural and urban, where such services were previously nonexistent. For years, their jobs have involved encouraging immunization and family planning, as well as treating basic illnesses.
“They have become the backbone of the primary health care services in this country,” said Ritu Priya Mehrotra, a professor of community health at the Jawaharlal Nehru University in New Delhi.
During the deadly waves of the coronavirus pandemic, these women — known by the acronym ASHA for accredited social health activist — were crucial in saving the lives of hundreds of thousands of coronavirus patients, officials at India’s Health Ministry say, by helping in the early detection of cases and spreading information on prevention. They were instrumental in countering vaccine hesitancy and helping India carry out one of the largest vaccination drives in the world.
Now, with the pandemic workload starting to slow down, these women, who say their work stretches for more than 14 hours a day and sometimes seven days a week, are protesting across the country over their meagre wages.
Regional governments pay the health workers around $40 a month, plus incentives. For example, there is a $4 bonus for every hospital childbirth they facilitate, and $1.50 for each full immunization of a child younger than 1.
They want a monthly salary of around $150, with incentives.
“Even when mortar shells land in villages, we work,” said Bimla Devi, who lives near the border between India and Pakistan in Jammu, where troops often trade gunfire. “When people are injured, you can’t tell them my job is only to look after women; you go and help.”
Dozens of the workers died during the pandemic after exposure to the coronavirus, in part because they lacked protective gear. One study of three Indian states by public health researchers at Oxfam in 2020 found that at least 25% of the health workers received no masks, and only 62% received gloves.
One worker, Geeta Devi, contracted COVID in a hospital, where she had accompanied a pregnant woman to deliver her baby in the northern state of Himachal Pradesh. After she became sick, her husband struggled to find her a bed.
“She died while helping people, without caring for herself,” said her husband, Rajvansh Singh.
Despite the risks, health workers across the country monitored coronavirus patients, provided medicine kits, isolated patients and sometimes delivered food to those in quarantine. Their most critical roles were ensuring continued access to essential health services when hospitals ran out of beds and encouraging vaccination.
Several women said they were beaten with sticks by angry villagers, who chased them away after rumors on social media that COVID vaccines had killed people or made them infertile.
“People were reading lies on social media, and we were motivating them to take vaccines,” said Seema Kanwar, who has done the job since 2006. “We told them we took the vaccine, and we did not die; how will you?”
India’s federal health ministry did not respond to emails seeking comment on the deaths of the health workers, the availability of protective gear and their demands for higher salaries. Prime Minister Narendra Modi has often lauded the health workers for their efforts to carry out government health plans at the grassroots level.
While the pandemic has been the focus for the past two years, the workers’ mandate was always broader than that, and now their attention is returning to general health issues affecting women and children.
Public health care infrastructure remains vastly underfunded in India, with a shortage of more than 600,000 doctors and 2 million nurses, according to a report by the Centre for Disease Dynamics, Economics & Policy, a research group based in Washington and New Delhi.
India, a country of 1.4 billion people, has a poor track record when it comes to health care, particularly of women and children. Malnutrition is widespread; infant and maternal mortality rates are high. Causes include poverty, poor access to doctors in rural areas, resistance to modern medicine and a deep-rooted denial of rights for women.
But health authorities have made remarkable strides recently in reducing death rates during childbirth. In March, the federal health ministry said the maternal mortality rate had dropped from 122 to 103 deaths per 100,000 births from 2015 to 2019. A United Nations-set target of bringing it down to 70 before 2030 now seems within reach.
As part of that effort, India introduced a health plan in 2005 that, among other things, introduced incentives for giving birth in a hospital.
But given both the difficulty of spreading the word in remote areas and widespread distrust of government programs, success would have been impossible without the health workers gaining the trust of their communities, experts said.
Every morning, Jadoun, a college graduate with a degree in history, leaves her house, sometimes veiling her face with her sari when men are around — a mark of respect in rural areas. She serves an area with a population running in the thousands.
At one house, she counselled a woman on birth preparedness; at another, she jotted down the name of a woman who had just learned she was pregnant. She will keep watch over her, give her iron tablets and register her name at a nearby public hospital.
“We are not only fighting superstition, but traditional practices too,” Jadoun said. “But when I look at zero deaths of women during childbirth and healthy people around, I feel proud about what we do.”
Anant Bhan, a public health researcher at Melaka Manipal Medical College in southern India, said the advantage of health workers living within the community has helped India deal with enormous gaps in delivering health services in the remotest corners of the country.
“The challenge is that ASHA workers are still seen as volunteers and expected to do a lot of work by the government, while not being adequately compensated,” he said.
One recent afternoon, Sunita Jain, another health worker in Rajasthan, walked through a narrow lane of mud and brick houses in a village there, Kolara. She was visiting Diksha Sharma, whose due date was drawing near.
Sharma said her husband wanted her to deliver her second child in a private hospital in a city dozens of miles away. Jain sought to convince her that giving birth in a nearby free public hospital was safe.
“Will you take care of me?” Sharma asked Jain. Her mother-in-law listened to the conversation carefully. (In rural India, mothers-in-law are often the deciders on childbirth questions.)
“We will not only take care of you, but I will go with you to the hospital and stay there,” Jain said. “Trust me, everything will be all fine, like the last time.”
-New York Times